 Huge amounts of compassion, planning, skill, innovation and professionalism have been going into the care and treatment of patients in COVID-19 ‘coloured areas’ in the Trust’s hospitals.
Huge amounts of compassion, planning, skill, innovation and professionalism have been going into the care and treatment of patients in COVID-19 ‘coloured areas’ in the Trust’s hospitals.
The coloured areas were brought in to ensure patient safety and to stop the spread of the virus on hospital sites. In the four areas of Blue, Yellow, Green Elective and Green, there are clear patient pathways designed by the Trust’s Infection Prevention Team to ensure that all staff follow rigorous safety guidelines and safe discharge procedures. Patients who are coming in for elective procedures and have been isolating are cared for in separate areas of all the main sites.
If a person has been shielding and has come urgently into hospital, then we aim to prioritise their care in a single room. The Trust is also working with volunteers from the local charity CancerCare who are taking cancer medications out to the homes of patients who are shielding.
• BLUE: COVID positive
• YELLOW: Suspected COVID
• GREEN: Non-COVID
• GREEN ELECTIVE: Non-COVID (elective shielded patients)
The Trust’s hospital areas are currently coloured as below:
Blue Area: This area is for patients who have tested positive for COVID-19. Patients can be at any stage of their treatment and can require Aerosol Generating Procedures (AGPs) for intubation or extubation. The patient can be recovered from COVID-19 and now symptom free. Staff in Blue Areas will wear an apron, gloves, fluid repellent surgical mask and facial protection (goggles/mask). When caring for patients with AGPs staff will also wear a filtering face piece respirator. The priority for single rooms is for patients who are shielding and patients who need AGPs. On discharge patients can go to their own home if they can maintain social isolation, social distancing and shielding (if necessary). If they are going to a place of care, the handover must confirm that they have been tested for COVID-19, that they are 14 days from the onset/testing date, symptom free for five days and have had discharge screening. For all patients leaving hospital a safe discharge is planned by the staff.
Yellow Area: Patients in Yellow Areas will have been assessed and have possible COVID-19. They may have been screened or are awaiting screening. They should not be positive for COVID-19. They can require any level of care including AGPs. Staff must wear an apron, mask, fluid repellent surgical mask and facial protection (goggles/visor). Staff treating patients needing AGPs must also wear a filtering face piece respirator. Priority in Yellow Areas for single rooms is given to patients on AGPs and who are shielding. Patients will move out of this area into a Blue Area if they test positive for COVID-19. On discharge the patient must be able to maintain isolating (if necessary), maintain social distancing and maintain shielding (if necessary).
Green Elective: The Green Elective Areas are for patients who have self-isolated in their homes for 14 days prior to admission. They will have been screened and no COVID-19 detected. Staff will wear an apron, gloves and fluid repellent surgical mask. Surveillance screening will continue during the patient’s hospital stay. All patients will have welfare checks prior to admission. When leaving hospital they must be able to maintain social distancing and shielding (if they are in this category). If a patient becomes symptomatic an assessment must be made by a clinician to confirm a diagnosis and other conditions should be considered. If confirmed, the patient should be moved to a Yellow Area as soon as possible.
Green Area: The Green Areas are for patients who have been assessed as having no current risk of COVID. Surveillance screening only is carried out in these areas. Staff will wear an apron, gloves and fluid repellent surgical mask. If a patient becomes symptomatic an assessment must be made by a clinician to confirm a diagnosis and other conditions should be considered.
Due to the changing numbers of those with COVID-19, there is a continuous review of care areas, which may mean the use of single patient rooms to accommodate a patient from a different colour stream.
As a result of the comprehensive safety measures designed within the Trust, we are minimising the risk of any hospital onset cases.
Since the beginning of May we have had two hospital onset definite cases and no probable cases.
For any hospital onset probable or definite cases a post infection review will be completed. This will be taken to the weekly Patient Safety Summit, with any themes and lessons learned shared appropriately.
In all areas of the Trust, Personal Protective Equipment (PPE) is worn by staff, however, hand hygiene remains fundamental to reducing transmission.
Patients are treated with the same care and compassion as on non-COVID wards and additional measures have been introduced to help patients stay in touch with their loved ones.
A huge amount of sympathetic care is being given by the Trust’s Chaplaincy Team and Bereavement Services who are ensuring that patients’ emotional needs are being looked after.
The Chaplaincy Team has been distributing special knitted hearts to bring comfort to hospital patients and family members.
 Deacon Deborah Wilde from the Chaplaincy Team has been distributing the hearts which have been lovingly hand-crafted by members of local churches. One heart is given to the patient and one to the relative who can’t be with them, whether at the end of life, or just when someone is missing their family.
Deacon Deborah Wilde from the Chaplaincy Team has been distributing the hearts which have been lovingly hand-crafted by members of local churches. One heart is given to the patient and one to the relative who can’t be with them, whether at the end of life, or just when someone is missing their family.
Currently, due to the risk of infection, the other hearts can’t be given directly to family members but are instead placed with patients’ belongings so that families can have them at a later date. The hospital team also makes sure that the hearts are left for a period of time before they are used and huge care is taken to prevent the spread of infection when given to patients following advice from the Infection Prevention Team.
The hearts are bringing a sense of comfort to people and many patients and family members have said they appreciate the caring gesture.
Another way in which patients in COVID-19 ‘coloured areas’ are receiving special support is through the use of iPad computers. Many of the iPads were donated to the Bereavement Team during the COVID-19 crisis.
The iPads have been used in COVID coloured areas to reassure patients and family members when they haven’t been able to see each other due to hospital visiting restrictions and need to isolate and/or shield.
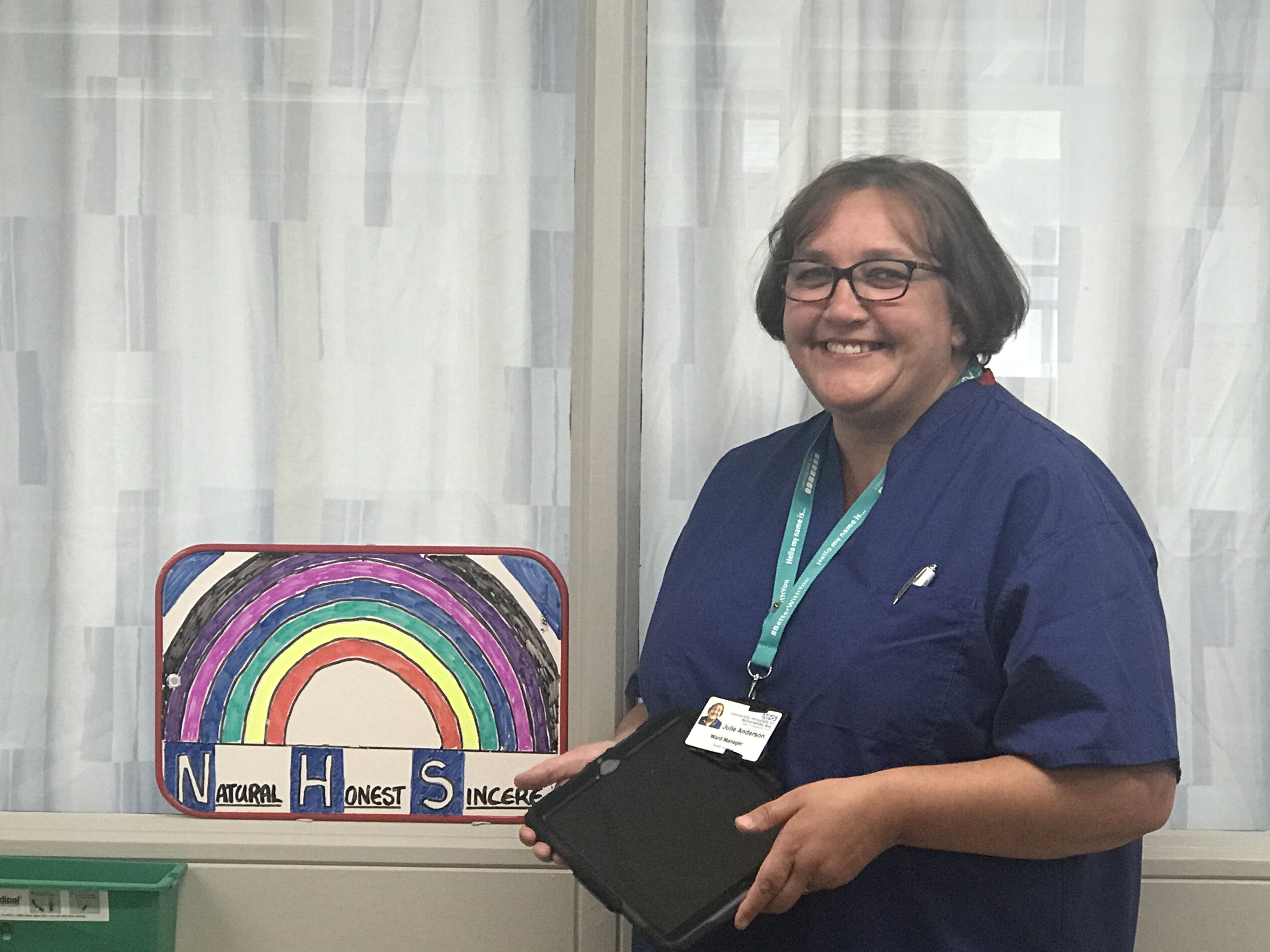
For example, on the Langdale Unit at Westmorland General Hospital in Kendal the team has been enabling patients and families to connect via the iPads.
Julie Anderson, the Ward Manager, has said the use of iPads has proved hugely positive. Julie explained that the iPads are helpful for families because they can see that their loved one is getting better. Seeing this on the iPad stops families worrying unnecessarily.
Patients with dementia and COVID-19, for example, can quickly become quite withdrawn and may not have seen their relatives for weeks due to the restrictions. The family and patient can all log on to the iPad at the same time to see each other and have a chat and in many cases, this is very effective. Risk assessments are carried out where a visit by a family member may be a requirement for the well-being of the patient and in this case, protective equipment is provided.
One patient, who was deaf, was able to see his wife talking to him on an iPad and it was a very joyous moment. The staff were able to translate what his wife was saying and he was very grateful. The patient said it was the best thing that had happened to him for a long time.
Staff have also been working behind the scenes doing special things for patients in the coloured areas such as having birthday celebrations and making bunting for VE Day. COVID-19 may have necessitated changes to safety procedures, but the unstinting compassion of the Trust’s staff remains the same.

