Here at UHMBT we are committed to improving standards of care across our services and to ensuring that the people of Morecambe Bay get the best care and experience possible.
Here at UHMBT we are committed to improving standards of care across our services and to ensuring that the people of Morecambe Bay get the best care and experience possible.
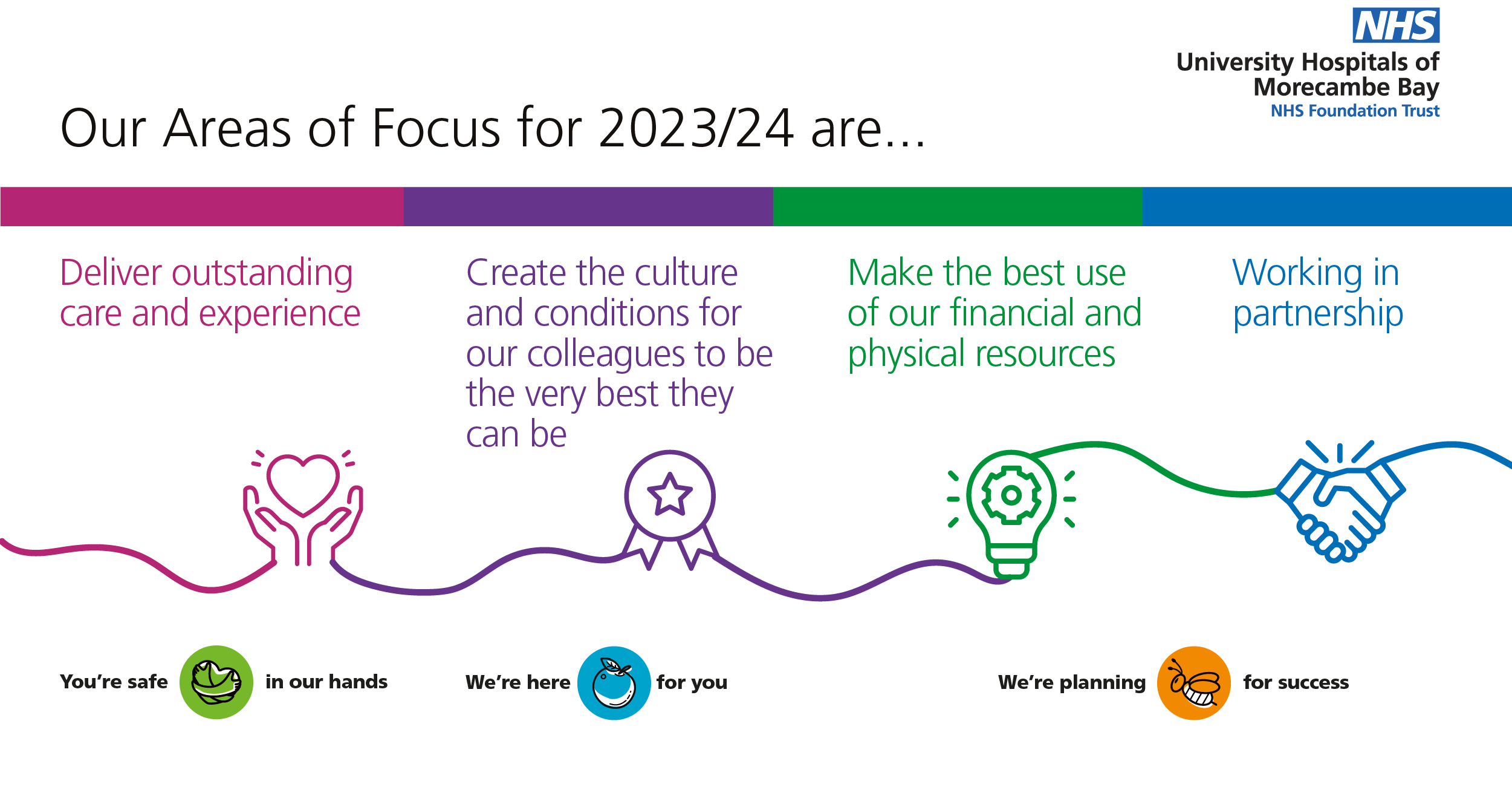
As a NHS Trust, it’s hugely important that we have a set of Trust Priorities that everyone supports so we can continue to provide safe and high-quality services.
This is why we have our Areas of Focus each year, to enable us to have a shared focus. In 2022, we launched our new Trust Strategy - Putting Patients First. The Areas of Focus are a vital part of how we will achieve what we have set out in the strategy, so for 2023/24, these now reflect our four strategic Trust Priorities.
One of our four Areas of Focus is: ‘Delivering Outstanding Care and Experience’.
Lynne Wyre, Deputy Chief Nurse for UHMBT, said “Over the last couple of years, we have taken forward several key priorities and objectives to improve and sustain our services for the benefit of our patients and local communities.
“This has been partly in response to external scrutiny from the Care Quality Commission (CQC) and NHS England and Improvement (NHS E/I), and also due to our commitment to continuous improvement.
“It’s important that we keep reminding ourselves of our Trust Priorities and Areas of Focus as well as remembering the individual objectives and actions we all have within our teams and Care Groups. It all comes down to putting patients first, being quality and safety driven and being clinically led.
“We want our patients to have the best possible care and experience, so we are making sure that we have the right people with the right skills and the right systems in place to provide excellent care.
“We are focusing on embedding a culture of continuous improvement and evidence-based practice across all our services to ensure that we truly learn from things that have gone well and from things that have not gone so well. As we move into a new system of governance, we will have more of an opportunity to do that.”
 We will:
We will:
- Improve access, standards of care and outcomes across all our services.
- Have plans in place to ensure the right people with the right skills are in the right place at all times to provide safe, high-quality care.
- Focus on embedding a culture of continuous improvement.
- Embed evidence-based practice across all services and ensure we have the processes in place to truly learn when we get things wrong.
We already have a system of Clinical Service Reviews in place which is well embedded, and the next step will be to introduce a Quality Accreditation Scheme.
Our Harm Free Care Panel meets on a weekly basis and links in with our governance processes in relation to reviews of clinical incidents and serious incidents.
 Likewise, our Mortality Reviews are enabling us to learn from deaths and to make improvements to our care and services. We are also working to improve patient flow and to transform our Outpatients Service.
Likewise, our Mortality Reviews are enabling us to learn from deaths and to make improvements to our care and services. We are also working to improve patient flow and to transform our Outpatients Service.
Lynne said: “Patient falls and pressure sores have been a huge focus over the last 12 months and I'm pleased to say we haven't had a Grade 3 or Grade 4 pressure sore since November 2022. There is still work to do, but this shows great progress.
“We've made huge improvements around our falls with moderate harms, and we will continue to work on that to improve care for our patients. Again, we will achieve this by having the right staff and with the right skills in the right place at the right time.
“We now have a system of bi-annual workforce reviews and each individual ward is taken into account. Each review is against a set of national workforce standards, and we report regularly to the board. We have had significant investment into our wards to create a safer environment and better experience for patients, families and colleagues.
“If we have the right processes and the right numbers of staff in the right place, it will improve colleagues’ experience, patient experience and hopefully reduce turnover and sickness rates.”
 To further develop and embed a culture of continuous improvement at our Trust, we've done a lot of work through the national Recovery Support Programme (RSP), and the next stage of that will be to establish a Transformation and Improvement Board. This new board will help us to monitor, sustain and embed our improvements.
To further develop and embed a culture of continuous improvement at our Trust, we've done a lot of work through the national Recovery Support Programme (RSP), and the next stage of that will be to establish a Transformation and Improvement Board. This new board will help us to monitor, sustain and embed our improvements.
There are six transformation schemes, each one with a one-year delivery plan. This involves patient flow throughout our entire system, transformation of our Outpatients Service and our Clinical Strategy. In essence, this means our organisation will be clinically-led and everyone can have an input. Our digital work will also be hugely important as we move to a new Electronic Patient Record (EPR) in the next few years.
We will continue to embed evidence-based practice and learning across all of services to make sure we have the right processes in place. Our Clinical Effectiveness forum will continue to ensure that we achieve compliance with national ‘Get it Right First Time’ (GIRFT) standards and the National Institute for Health and Care Excellence (NICE) standards.
The Forward Audit Plan, which is aligned to risks and issues, requires each and every one of us in our Care Groups and services to identify improvements that we can actively monitor. We are moving from our current way of reviewing clinical incidents and serious incidents to the new the Patient Safety Incident Response Framework (PSIRF).
 This will increase our learning from the experience of our patients because we will involve patients and families in the incident review process. It won't just be a clinical opinion - it will be very much about how things feel for the person who was involved in the incident. We hope this will mean our patients will feel listened to, and it's key that we learn from their feedback as well.
This will increase our learning from the experience of our patients because we will involve patients and families in the incident review process. It won't just be a clinical opinion - it will be very much about how things feel for the person who was involved in the incident. We hope this will mean our patients will feel listened to, and it's key that we learn from their feedback as well.
Lynne added: “There are so many people who have been involved in the improvements over the last two years – the Trust feels like a very different place to work and I hope that patients feel the difference too.
“I would like to thank all of the teams that have been involved in all of the quality improvement work. It has been a really exciting time.
“What we need to do now is sustain and embed our improvements and I’m sure that everybody is committed to doing that. Thank you to everybody for all of your hard work – it really is making a difference!”