Having a gastroscopy
You have been advised to have an endoscopy to help find the cause of your symptoms. The test is sometimes called a gastroscopy or endoscopy. This information has been prepared after talking to patients who have had the test. It may not answer all your questions, so if you have any worries please don't hesitate to ask. The endoscopy staff will be available to answer any queries.
What is a Gastroscopy?
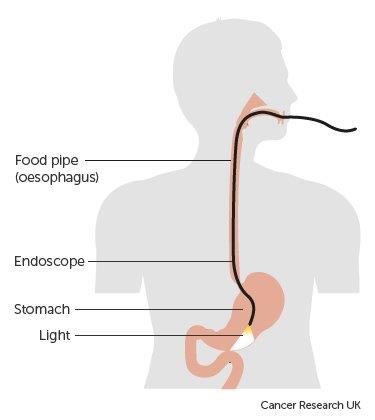
Gastroscopy is a test which allows the endoscopist to look directly at the lining of the oesophagus (gullet), the stomach, and the first part of your small bowel called duodenum. This is done with a long flexible tube with a bright light on the end. The camera shows a video image onto a screen and allows the endoscopist to check if any disease is prevent. The endoscopist may take pictures and/or biopsies which are sent to the labratory for analysis. The tissue sample (biopsy) is removed painlessly through the gastroscope using tiny forceps.
What should I expect?
The preparation:
To allow a clear view the stomach must be empty. You will be asked to have nothing to eat for six hours before your test. You will be allowed to drink clear fluids until two hours before your test.
What happens when I arrive?
Once you have booked in to reception you will be met by a qualified nurse who will give you a brief medical assessment to establish your medical condition and any relevant past surgery or illness. Your blood pressure, heart rate and oxygen levels will be recorded. The nurse will ensure that you understand the procedure and discuss any concerns or questions that you may have.
If you are happy to proceed you will be asked to sign a consent form before your procedure starts.
Please be prepared to be in the department for the full morning or afternoon depending on your appointment time. Wear loose comfortable clothing.
During the procedure:
In the examination room you will be asked to remove any false teeth immediately before the procedure and they will be kept safely until after the examination. You will be made comfortable on a hospital trolley, laying on your left side. A nurse will be with you throughout the procedure which usually takes no more than five minutes.
In order to keep your mouth open, a plastic mouth guard will be placed between your teeth. The endoscopist will pass the gastroscope into your stomach; it will not cause any pain or affect your breathing at any time. During the procedure air is passed through the endoscope to distend your stomach to allow clearer views. The air is sucked out of your stomach at the end of the test. If you get a lot of saliva in your mouth the nurse will use suction to clear it. When the examination is finished the endoscope is removed quickly and easily. There are two ways in which the test can be done:
Method 1: No sedation – the throat is numbed with a local anaesthetic spray. You will be wide awake throughout the procedure. You will be able to talk to the endoscopist immediately after the test and you will be given something to eat and drink 30 minutes after the throat spray. You will be able to drive home, return to work or go about your day as usual.
Method 2: Intravenous sedation – the sedation will be administered into a vein in your arm or hand. This will make you feel drowsy and relaxed but not unconscious, and therefore you will still hear what is happening around you. If you are having sedation you will be given oxygen through a sponge in your nose. The sedation can make you forgetful so you may not remember the procedure afterwards.
After the test:
You will be required to lie on a hospital trolley or sit in a chair after the procedure to recover from the sedation or wait for the throat spray to wear off. You may feel a little bloated if any air is left in your stomach or you may experience a sore throat. Both these discomforts will pass and require no medication. You will be given something to eat and drink before you are discharged. One of the nurses or doctors will go through the findings of your endoscopy with you and discuss any follow up or treatment that you may require. We also write this down for you to take home as a reminder.
Going home:
If you have had sedation it is important that you are collected from the Endoscopy unit and are driven home by a relative or friend who will need to stay with you for 24 hours. You must not go back to work, drive, operate machinery, drink alcohol or make any important decisions for 24 hours after the sedation.
Having had sedation you may feel fully alert after your gastroscopy, however the drug remains in your system for 24 hours and you can intermittently feel drowsy with lapses in memory. You are able to resume normal activities straight away if you have not had sedation, or after 24 hours following sedation.
When do I know the results?
You will be informed of any results of your procedure when you are discharged. You will also be told of any follow up or recommendations following the procedure. If you have biopsies, the results will be sent to your referring doctor and to your G.P between two and six weeks depending on your referral. If you have had sedation you may wish to have a relative with you on discharge as you may not recall the information given due to the sedation having made you forgetful.
Are there any risks involved?
A gastroscopy is a safe procedure and the risk of any complication is minimal.
There is a small risk of reaction to the sedation which can occasionally cause problems with breathing, heart rate and blood pressure. If any of these problems do occur they are normally short lived. Careful monitoring by a trained endoscopy nurse ensure that any potential problems can be identified and treated rapidly.
There is a small risk of causing a tear or perforation to the lining of your gullet or stomach or bleeding which could mean you being admitted to hospital. Certain cases are treated with antibiotics and intravenous fluids. Some may require surgery.
It is important that you follow the fasting instructions so that your stomach is empty prior to your gastroscopy. If there is food or fluid in your stomach there is a risk that you may vomit and inhale any fluid and cause an aspiration pneumonia.
There is also a small risk of damage to teeth or bridge work and you may experience a sore throat following the procedure.
Are there any alternatives?
Gastroscopy is considered the best test to examine the stomach, which also allows tissue samples to be taken. A barium meal x-ray can be done as an alternative. This involves swallowing barium liquid and x-ray pictures being taken, but does not allow tissue samples to be taken.
Checklist:
- Please let us know if you cannot attend your appointment, so we can allocate it to someone else.
- Bring an up to date list of medications.
- Please contact us if you take Warfarin, Clopidogrel, Rivaroxaban, Dabigatran, Apixaban or any other blood thinning tablets.
- If you take insulin or tablets for your diabetes you should contact your practice/diabetic nurse for advice.
- Write down any concerns/questions.
- If you need information in your own language or an interpreter, including sign language, please contact the endoscopy unit.
- Ensure one finger is free of nail polish or false nails.
- If you are having sedation make sure that you have someone to collect you in a car/taxi and to stay with you for 24 hours following the procedure.
If you have any problems or need advice you can contact the endoscopy team for advice:
- FGH and WGH Mon - Fri 9am - 6pm
- RLI open 7 days, 9am - 6pm
Alternatively you can contact your GP.
The numbers to call are:
Furness General Hospital: telephone 01229 491112
Royal Lancaster Infirmary: telephone 01524 583724
Westmorland General Hospital: telephone 01539 715175
A useful website to look at is www.corecharity.org.uk.

